The intricate relationship between the gut and the brain has long fascinated researchers and health professionals alike. Emerging evidence suggests that disturbances in gut health may play a significant role in the development and progression of various neurological disorders. In this article, we’ll delve into the fascinating field of gut-brain communication, exploring the potential links between gut health and neurological conditions such as Alzheimer’s disease, Parkinson’s disease, depression, and anxiety. By understanding this complex interplay, we can uncover new avenues for both prevention and treatment of neurological disorders.
The Gut-Brain Axis
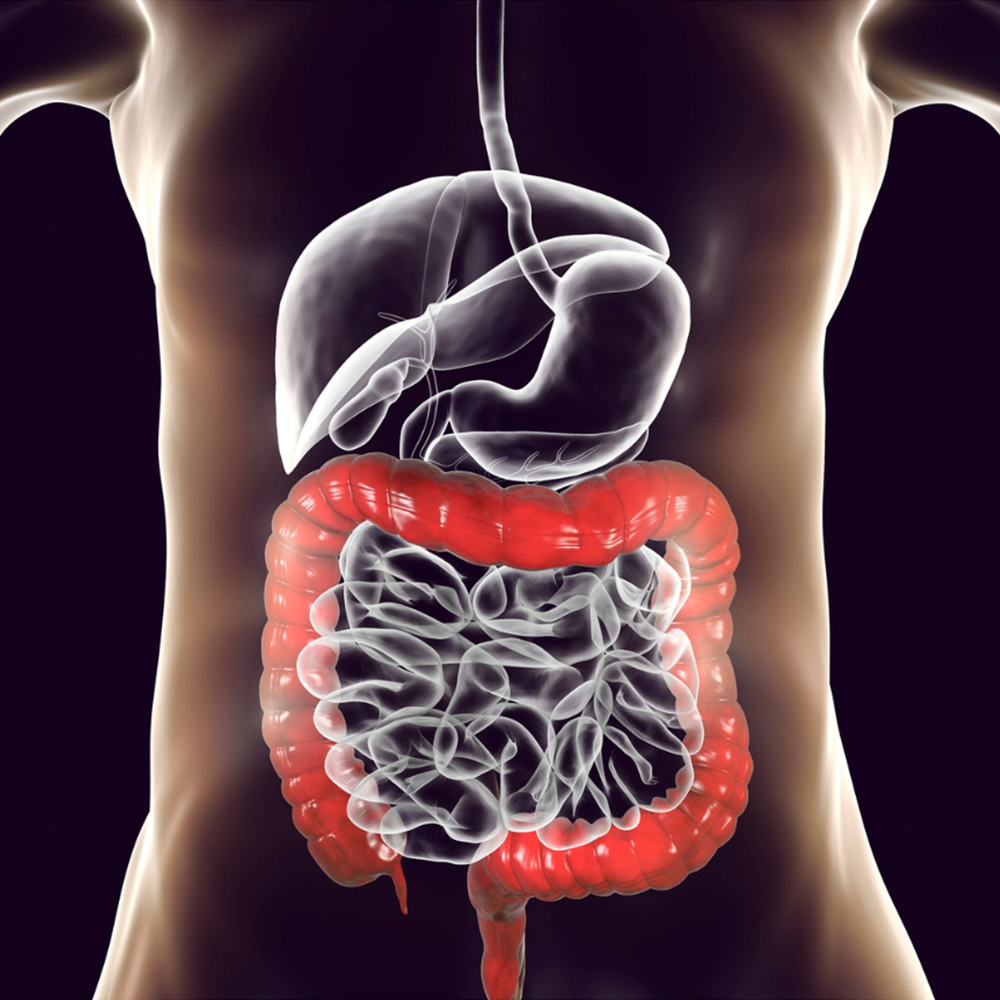
The gut-brain axis denotes the two-way communication network linking the gastrointestinal tract with the central nervous system. This communication occurs through various pathways, including the vagus nerve, neurotransmitters, hormones, and immune system molecules. The gut is home to trillions of microorganisms collectively known as the gut microbiota, which play a crucial role in maintaining gut health and modulating brain function. Disruptions in the gut microbiota composition, known as dysbiosis, have been implicated in the pathogenesis of neurological disorders.
Alzheimer’s Disease
Alzheimer’s disease, the most common form of dementia, is characterized by the accumulation of amyloid-beta plaques and tau tangles in the brain, leading to cognitive decline and memory loss. Emerging research suggests that alterations in gut microbiota composition and function may contribute to the development and progression of Alzheimer’s disease. Dysbiosis, intestinal permeability (leaky gut), and systemic inflammation are thought to promote neuroinflammation and the accumulation of pathological proteins in the brain.
Parkinson’s Disease
Parkinson’s disease is a progressive neurological disorder characterized by the loss of dopamine-producing neurons in the brain, leading to motor symptoms such as tremors, rigidity, and bradykinesia. Mounting evidence suggests a potential link between gut health and Parkinson’s disease, with studies demonstrating alterations in the gut microbiota composition of individuals with Parkinson’s disease compared to healthy controls. Alpha-synuclein, a protein implicated in Parkinson’s pathology, may travel from the gut to the brain via the vagus nerve, triggering neuroinflammation and neuronal damage.
Depression
Depression is a common mood disorder characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities. Growing evidence suggests a bidirectional relationship between gut health and depression, with alterations in gut microbiota composition observed in individuals with depression. The gut microbiota produces neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), which play a key role in mood regulation. Dysbiosis and intestinal inflammation may contribute to changes in neurotransmitter levels and mood disturbances.
Therapeutic Interventions
Targeting gut health may represent a promising therapeutic approach for the prevention and management of neurological disorders. Strategies to promote gut health include dietary modifications, probiotic and prebiotic supplementation, faecal microbiota transplantation (FMT), and lifestyle interventions such as stress reduction and regular exercise. By restoring gut microbiota balance and reducing intestinal inflammation, these interventions may help alleviate symptoms and improve outcomes in individuals with neurological disorders.
Overview
The field of gut-brain research has revealed intricate connections between gut health and neurological disorders. Dysbiosis, intestinal permeability, and systemic inflammation are emerging as key contributors to the pathogenesis of conditions such as Alzheimer’s disease, Parkinson’s disease, depression, and anxiety. By understanding the complex interplay between the gut and the brain, we can identify new targets for intervention and develop innovative therapeutic strategies to promote neurological health and well-being. As research in this field continues to evolve, harnessing the power of the gut-brain axis holds great promise for improving outcomes and enhancing the quality of life for individuals affected by neurological disorders.